Thyroid hormones are “Goldilocks” hormones: the dose has to be “just right” for us to feel optimal. Doses that are too high or too low can result in symptoms.
I get tons of messages from people who report that they had begun to feel hypothyroid symptoms after having their thyroid medications reduced, based on a faulty lab interpretation.
One lady began to lose her hair in clumps; another became nearly bedridden!
Upon reviewing their labs and history, I realized that both had something in common: they had been feeling great on a regimen of T4 and T3 medications, but were found to have low TSH levels, which suggests hyperthyroidism or thyroid medication overdosing.
This finding prompted their doctor to reduce their medications.
To prevent this from happening, I recommend doing a full thyroid panel to get the full picture of what’s going on with an individual’s thyroid function. In order to get accurate lab tests, however, there are several factors that should be taken into consideration.
This article presents an in-depth discussion on:
- Recommended thyroid lab tests (and WHEN to test for accurate results)
- How to get accurate results with T4, T3, and T4/T3 combination medications
- Supplements and medications that may affect lab results
- What to do if you get a questionable lab result
Recommended Lab Tests
When first initiating treatment with thyroid medications for hypothyroidism, guidelines recommend testing thyroid function about four to six weeks after the start of the treatment, to determine if the dose of medication is correct. It may be prudent to run these tests sooner and more often if a patient is experiencing symptoms of hypothyroidism, hyperthyroidism, or both.
In addition to looking out for symptoms of hypo- or hyperthyroidism, I also recommend monitoring thyroid levels regularly to ensure the medication dose is still appropriate.
I recommend the following thyroid tests to measure your response to medications:
- TSH (Thyroid Stimulating Hormone) – TSH is a pituitary hormone that responds to low or high amounts of circulating thyroid hormone. People with Hashimoto’s and central hypothyroidism (a rare type of hypothyroidism) may have a normal reading on this test. In advanced cases of Hashimoto’s and primary hypothyroidism, this lab test will be elevated, as the body will signal the production of more TSH to cope with the lack of thyroid hormone. (Read this post about interpreting the TSH test for more information.) In Graves’ disease and hyperthyroidism, TSH levels will be low.
- Optimal reference range: between 0.5-2 μIU/mL
- Free T3 and Free T4 – Triiodothyronine (T3) is our primary biologically active thyroid hormone. About 20 percent of our T3 hormone comes from thyroid secretion directly, while the remaining 80 percent is produced when the thyroid hormone thyroxine (T4) is naturally converted to T3 within our bodies. While T4 is 300 percent less biologically active than T3, it is critical to our body’s ability to produce adequate and healthy levels of the needed T3. T3 is sometimes called our “go” hormone because it tells our body to boost metabolism, grow hair, and create more energy. Free T3 and T4 tests measure the levels of active thyroid hormone circulating in the body. When T3 and T4 levels are low, but TSH tests are in the normal range, this may lead your physician to suspect central hypothyroidism.
- Optimal T4 reference range: 15-23 pmol/L
- Optimal T3 reference range: 5-7 pmol/L
If your doctor does not order these tests for you, you can pay out of pocket and order them yourself through an independent lab network like Ulta Labs.
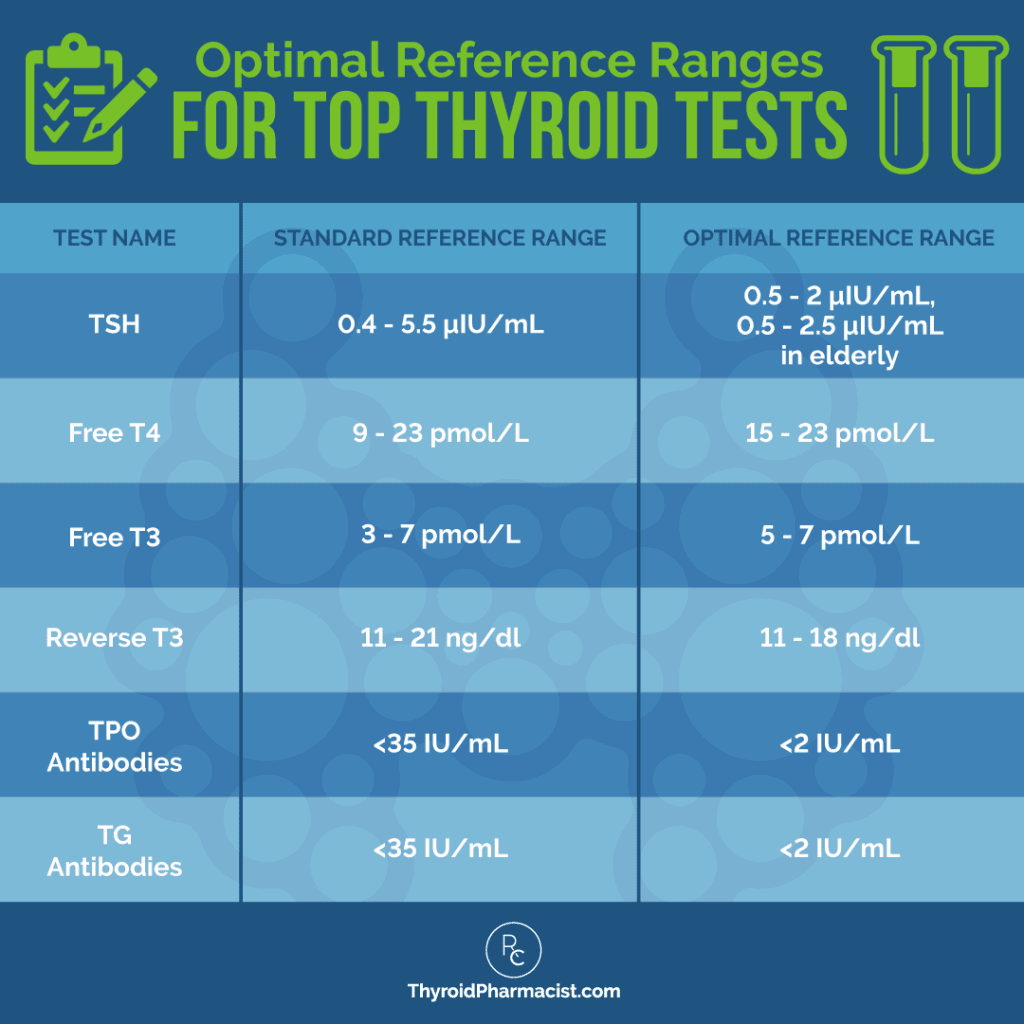
If your thyroid labs appear to be within the “normal” conventional ranges, but are not in the optimal reference ranges as noted above, you may still experience thyroid symptoms. (You can learn more about each of these tests and optimal ranges in my article on the top tests for diagnosing and monitoring Hashimoto’s.)
Please note, however, that depending on the type of thyroid medication you are taking, you may need to time your lab draw and intake of thyroid medication, in order to ensure you get the most accurate lab results. (More on that in a minute!)
Optimizing Thyroid Medication Absorption
Before we talk about timing your lab draw, let’s review how to take thyroid medications for proper absorption.
I recommend that you take your medication consistently at the same time each day, with a glass of water, at least 30 minutes before food. (Most doctors and pharmacists recommend taking them in the morning, upon waking.) Avoid taking acid reflux medications, magnesium, calcium, and iron supplements within four hours of taking thyroid medication, as they can impair thyroid medication absorption.
Absorption may also be impaired by foods such as soybean, cottonseed, walnuts, and fiber.
Beverages (not including water) can impair absorption as well. Of note, coffee can reduce the absorption of T4 in the intestines. (The T4 medication Tirosint may be an exception to this — please see my Tirosint article for more information.)
However, hot lemon water is an exception. Taking your thyroid medication with hot lemon water can offer the acidity needed to aid absorption (and is also great for helping the liver to detox).
Timing Thyroid Medications for Optimal Lab Results
Optimally absorbing your thyroid medication will help to ensure the body is getting adequate thyroid hormone, and may improve results when you do test your labs. However, even if you are getting adequate thyroid hormone and the body is absorbing it, there are factors that may lead to abnormal lab results, and steps you can take that will ensure accuracy.
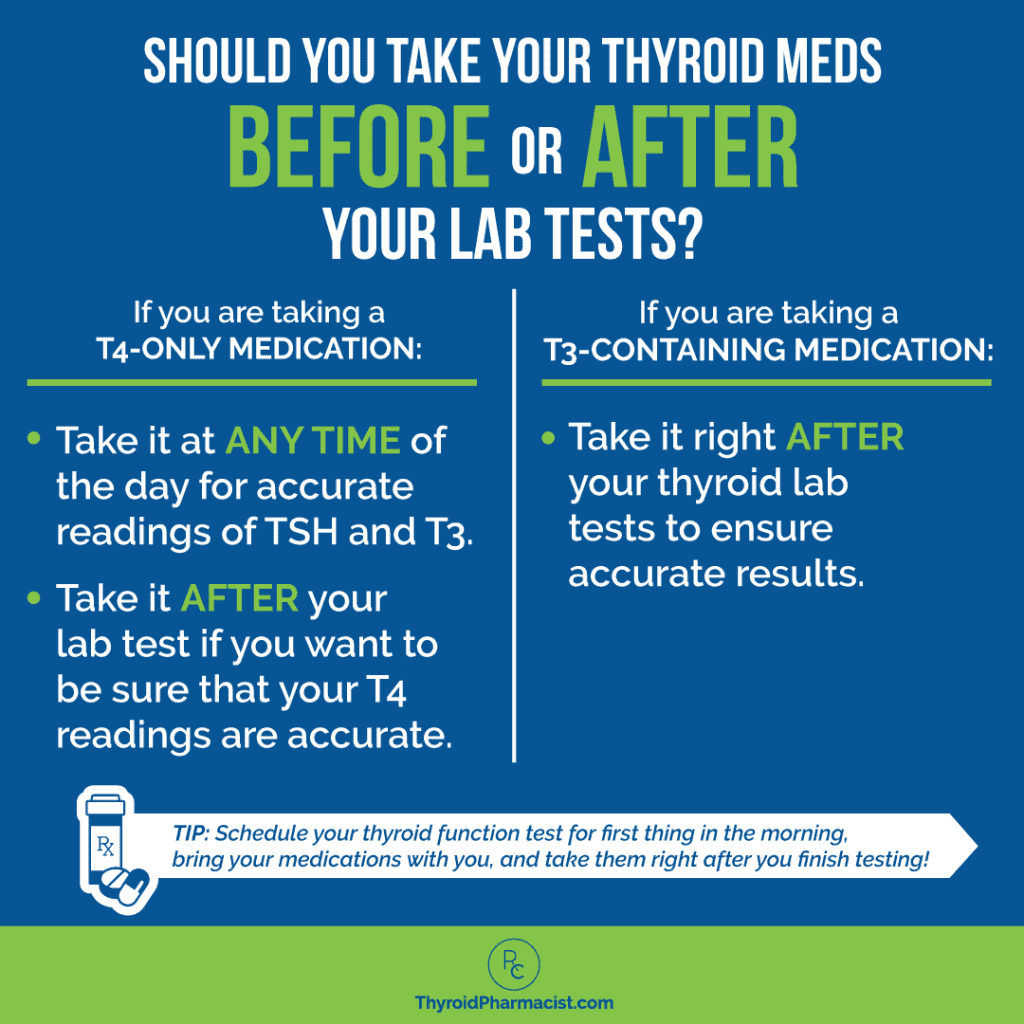
The first step to consider is when to take thyroid medications, if you are planning on heading to the lab. The timing of your thyroid medication may affect the accuracy of your thyroid test results, depending on what type of thyroid medication it is.
The recommendations for timing thyroid meds differ depending on the type of medication you take. Let’s dive into the recommendations for each type of medication.
Recommendations for Those on T4-Only Medications
T4-only medication (such as Synthroid, Levoxyl, Tirosint, Eltroxin, and generic levothyroxine) has a five- to nine-day half-life, which means that once you have become stable on the current dosage, it can take up to nine days for 50 percent of the dose to clear the body. T4 has a slow and steady release and won’t produce many fluctuations that can make a person feel like they’re on a thyroid roller coaster.
Whether you take your T4 medication right before your lab tests or haven’t taken it for up to 48 hours, your TSH value should be the same. Thus, you will get an accurate representation of your TSH value whether or not you take your T4 medication before a lab test.
The same goes for free T3 levels when you take a T4 medication. The free T3 level will also be relatively constant.
Levels of free T4, however, will peak two hours after your T4 medication is taken.
So let’s say you take your T4 medication at 8 am and have your blood test at 10 am – your thyroid labs may show that your T4 is falsely elevated. This may result in your doctor lowering your medication, when in reality, your T4 levels may be within range for the rest of the day, with the exception of that two-hour, post-dose peak.
In most cases, taking a T4 medication the morning before your lab test will not be an issue, as most doctors adjust the dosages according to the TSH, which stays stable after T4 dosing.
However, to get a reading of your T4 levels that is reflective of most of the day, you would want to postpone your T4 medication until after the lab test.
Thus, when taking T4-only medications, I generally recommend delaying your thyroid medications until after your lab test. For best results, schedule your thyroid labs early in the morning, and bring your thyroid medications to the appointment to take them right after the lab draw.
Recommendations for Those on T3-Containing Medications
If you’re taking a T3-containing medication (such as Cytomel or liothyronine) to optimize your free T3 levels, the timing of your tests matters.
Right after a dose of T3-containing medications, free T3 levels tend to rise, then peak at around the four-hour mark.
T3 has a typical half-life of 18 hours to three days. That means it could take less than a day for T3 levels to start rapidly declining in your body!
So, if you were to take a T3-containing thyroid medication a few hours before your thyroid lab tests, your lab results might show that you have too much T3, even when you may be accurately dosed. Or, they may be in the normal range, when you are actually under-dosed.
T3-containing medications can also temporarily alter TSH levels. Researchers who monitored the levels of TSH, free T3, and free T4 in people with hypothyroidism who were taking combination (T3/T4-containing) medications over a 24-hour period, found that TSH levels may be falsely suppressed.
This is because, right after taking a T3-containing medication, TSH levels drop and stay suppressed for around five hours. TSH levels will then increase until around 13 hours post-dosage, where levels will stabilize.
So in order to get an accurate reading of your TSH levels on a T3-containing medication, you would need to wait at least 13 hours after taking your T3-containing medications before testing!
Again, for this reason, I generally recommend delaying your thyroid medications until after your lab test. For best results, test thyroid labs early in the morning, and bring your thyroid medications to the appointment to take them right after the lab draw.
Recommendations for Those on T4/T3 Combination Medications
If you’re taking a combination medication that contains both T4 and T3 (such as Armour, Nature-Throid, WP Thyroid, or compounded T4/T3), the timing of your tests does matter and may make a huge difference in getting you on an appropriate medication dose.
As mentioned above, taking any medication with T3 will first drop TSH levels for around five hours before they start rising again. Thus, it is usually best to postpone taking your T4/T3 combination medication until after you get your lab tests done.
So again, with this medication type, I recommend getting your thyroid function tests done first thing in the morning before taking your medications, bringing your medications with you, and taking them right after you complete your thyroid tests, to ensure that you get the most accurate lab results.
*Please note: The half-life of T4/T3 combination medications may vary per formulation (this can vary depending on the formulation and whether it is an immediate or sustained release version), so some people may have a falsely suppressed TSH, even at the euthyroid state (or the state of normal thyroid function), when taking T3-containing medications.
This is when free T3 and T4 testing will come in handy, as thyroid health can be assessed through optimal levels of free T3 and free T4. Thyroid health can also be determined by assessing one’s list of symptoms.
Supplements and Medications That May Interfere with Thyroid Lab Results
It’s important to note that there are some supplements and medications that can interfere with lab results, that you should be aware of before getting thyroid lab work done:
- Biotin — The American Thyroid Association recommends that patients stop taking biotin for at least two days before a TSH test. Biotin can result in falsely high levels of T4 and T3, and falsely low levels of TSH on lab results. Biotin supplements (taken at 5-10 mg/day) can interfere with thyroid labs and cause a false appearance of hyperthyroidism. There are case reports of people taking biotin and having low TSH, high T4, high T3, and elevated TSH-receptor antibodies (in the absence of hyperthyroid or Graves’ symptoms) show up on lab results. That said, lab values do normalize after seven days of being off biotin. If you’re going in for a thyroid lab draw, skip the biotin for two days beforehand, to ensure that it doesn’t interfere with the results.
- Supplements containing estrogenic compounds — Supplements that contain estrogenic compounds such as soy, can lead to falsely elevated TSH levels. However, please note that I do not recommend products containing soy to those with Hashimoto’s, as it is one of the most common food sensitivities seen in those with the condition.
- Medications that interfere with thyroid test results — In addition to supplements, there are certain medications that can interfere with thyroid lab test results and may lead to false readings. This type of interaction is known as a drug-lab interaction, and two common types of medications that interfere with thyroid labs include:
- Glucocorticoids, dopamine, dobutamine, and octreotide – These can lower TSH without indicating true thyroid dysfunction.
- Certain NSAIDs (nonsteroidal anti-inflammatory drugs) of the salicylate subclass (specifically, salsalate, diclofenac sodium, and naproxen) – These have been found to decrease serum T3 and T4 measurements.
- Drug-drug interactions — False alterations of thyroid labs are not to be mistaken with drug-drug interactions, which occur between thyroid hormones and certain medications, and lead to actual changes in thyroid hormone levels. Simply stated, there are medications that interfere with thyroid lab results by actually interfering with thyroid hormone function — this means they cause real alterations in thyroid hormone levels. Some of these alterations are clinically significant and may require a dose adjustment of your thyroid medications when taking the two medications concurrently. I’m working on a separate article that goes in depth about these medications, so stay tuned!
What to Do if You Get a Questionable Lab Result
If you feel that you may have received an inaccurate lab result (perhaps you’ve realized the timing of your thyroid medication may have interfered with its accuracy), there are steps you can take to receive a more accurate result.
First, try to determine if the timing of your medication in relation to your thyroid lab tests could be a factor. Writing down the details about timing and dosages of medications may help pinpoint if and/or how your thyroid medication may have affected your lab result(s). It may also be helpful to determine if you consumed additional medications and/or supplements mentioned previously, around the time of your thyroid testing.
If you find that the timing of your medications and/or other factors mentioned in this article did indeed lead to inaccurate lab results, it may be necessary to retest.
Retesting may involve some planning around when you take your thyroid medications, and possibly delaying other medications and/or supplements by a few hours, so that there is no interference when you do draw your labs.
If after receiving accurate results, you still feel hypothyroid, are still experiencing debilitating symptoms, or if your lab results do not fall within the optimal ranges (as discussed earlier in this article), be sure to re-read the “Optimizing Thyroid Medication Absorption” section of this article (above) to ensure you are taking your thyroid meds away from foods that can inhibit their absorption. If you are, then it may be time to have a conversation with your doctor about adjusting your medications.
This may involve:
Please note, however, that there have been recalls in the past, so make sure to discuss this with your doctor, and check out this article on thyroid medications to review all available options on the market. While trying to get on the right dosage of medication, you will want to test your thyroid labs every four to six weeks to ensure your labs are within range.
Once you become stabilized on your new thyroid medications, you can start testing thyroid levels every three months to one year for ongoing monitoring.
I have a free, downloadable eBook, Optimizing Thyroid Medications, that provides further guidance on this optimization process.
Next Steps
As mentioned above, if you are following all the steps for accurate lab results but they are still coming back abnormal, talk to your doctor about a dosage adjustment.
I recommend that you also investigate the possibility that something else is interfering with the absorption of your thyroid medication, such as fillers like gluten, or certain supplements that you are taking.
While some supplements can result in false readings of thyroid levels, others reflect a true change in thyroid levels — this change may be an improvement or worsening of levels depending on the supplement. Examples of such supplements include aloe vera, cordyceps, vitamin A, and ashwagandha, which all lower TSH. (I’m working on an article on supplements that can help lower TSH naturally — stay tuned!)
In addition to medications that cause false alterations in thyroid lab results, there are also medications that have actual drug interactions with thyroid hormones, and the altered labs are a real reflection of how the addition of a new drug impacts the activity of thyroid hormones in the body.
In my training as a pharmacist, I learned that there are some medications that have a multitude of drug interactions — one of these medications is thyroid hormone! Some of these drug interactions may be clinically significant, meaning that they can alter the absorption, distribution, metabolism or elimination of the thyroid hormones, necessitating a dosage change in thyroid hormones while the person is taking both medications.
A person who has been stable on thyroid medications but begins experiencing symptoms of hypo- or hyperthyroidism following the addition of a new medication, should inquire about potential drug interactions and request lab tests.
I’ll be sharing more information about significant drug interactions with thyroid hormones in the future, but for now, I recommend checking with your pharmacist whenever you start a new medication, to see if your dose of thyroid medication needs to be adjusted.
In summary, receiving accurate results is important to ensure no ineffective changes are made to your current medications, and to assess how your thyroid is currently functioning. Once you’ve identified and addressed things that could be affecting your TSH or T4 lab results, consider retesting with the proper timing of medications and/or supplements for accuracy.
I hope this helps you on your healing journey!
P.S. You can download a Thyroid Diet Guide, 10 thyroid-friendly recipes, and the Nutrient Depletions and Digestion chapter of my first book for free, by signing up for my weekly newsletter! You will also receive occasional updates about new research, resources, giveaways, and helpful information.
For future updates, make sure to follow us on Facebook, TikTok and Instagram, too!
References
- Saravanan P, Siddique H, Simmons D, Greenwood R, Dayan C. Twenty-four Hour Hormone Profiles of TSH, Free T3 and Free T4 in Hypothyroid Patients on Combined T3/T4 Therapy. Experimental and Clinical Endocrinology & Diabetes. 2007;115(04):261-267. doi:10.1055/s-2007-973071.
- Food and Synthroid Drug Interactions. Drugs.com. https://www.drugs.com/drug-interactions/lemon-with-synthroid-2993-0-1463-869.html. Accessed June 9, 2021.
- American Thyroid Association. https://www.thyroid.org/patient-thyroid-information/ct-for-patients/vol-1-issue-1/vol-1-issue-1-p-21/. 1(1):21. Accessed June 10, 2021.
- Dong BJ. How medications affect thyroid function. West J Med. 2000;172(2):102-106. doi:10.1136/ewjm.172.2.102
- Ardabilygazir A, Afshariyamchlou S, Mir D, Sachmechi I. Effect of High-dose Biotin on Thyroid Function Tests: Case Report and Literature Review. Cureus. 2018;10(6):e2845. Published 2018 Jun 20. doi:10.7759/cureus.2845
- Clark CD, Bassett B, Burge MR. Effects of kelp supplementation on thyroid function in euthyroid subjects. Endocr Pract. 2003;9(5):363-369. doi:10.4158/EP.9.5.363
- Otun, J., Sahebkar, A., Östlundh, L. et al. Systematic Review and Meta-analysis on the Effect of Soy on Thyroid Function. Sci Rep. 2019;9(3964). https://doi.org/10.1038/s41598-019-40647-x
- Koulouri O, Moran C, Halsall D, Chatterjee K, Gurnell M. Pitfalls in the measurement and interpretation of thyroid function tests. Best Pract Res Clin Endocrinol Metab. 2013;27(6):745-762. doi:10.1016/j.beem.2013.10.003
- Bishnoi A, Carlson HE, Gruber BL, Kaufman LD, Bock JL, Lidonnici K. Effects of commonly prescribed nonsteroidal anti-inflammatory drugs on thyroid hormone measurements. Am J Med. 1994;96(3):235-238. doi:10.1016/0002-9343(94)90148-1
- Liewendahl K, Majuri H, Helenius T. Thyroid function tests in patients on long-term treatment with various anticonvulsant drugs. Clin Endocrinol (Oxf). 1978;8(3):185-191. doi:10.1111/j.1365-2265.1978.tb01493.x
- De Luca F, Arrigo T, Pandullo E, Siracusano MF, Benvenga S, Trimarchi F. Changes in thyroid function tests induced by 2 month carbamazepine treatment in L-thyroxine-substituted hypothyroid children. Eur J Pediatr. 1986;145(1-2):77-79. doi:10.1007/BF00441860
- Cooper JG, Harboe K, Frost SK, Skadberg Ø. Ciprofloxacin interacts with thyroid replacement therapy. BMJ. 2005;330(7498):1002. doi:10.1136/bmj.330.7498.1002
- Trifiro G, Parrino F, Sultana J, et al. Drug interactions with levothyroxine therapy in patients with hypothyroidism: observational study in general practice. Clin Drug Invest. 2015;35(3):187-195.
- Irving SA, Vadiveloo T, Leese GP. Drugs that interact with levothyroxine: an observational study from the Thyroid Epidemiology, Audit and Research Study (TEARS). Clin Endocrinol (Oxford). 2015;82(1):136-141.
- Liwanpo L, Hershman JM. Conditions and drugs interfering with thyroxine absorption. Best Pract Res Clin Endocrinol Metab. 2009;23(6):781-792.
- Sachmechi I, Reich DM, Aninyei M, Wibowo F, Gupta G, Kim PJ. Effect of proton pump inhibitors on serum thyroid-stimulating hormone level in euthyroid patients treated with levothyroxine for hypothyroidism. Endocr Pract. 2007;13(4):345-349. doi:10.4158/EP.13.4.345
- McConnell RJ. Abnormal thyroid function test results in patients taking salsalate. JAMA. 1992;267(9):1242-1243.
- Aanderud S, Myking OL, Strandjord RE. The influence of carbamazepine on thyroid hormones and thyroxine binding globulin in hypothyroid patients substituted with thyroxine. Clin Endocrinol (Oxf). 1981;15(3):247-252. doi:10.1111/j.1365-2265.1981.tb00662.x
- Isojärvi JI, Turkka J, Pakarinen AJ, Kotila M, Rättyä J, Myllylä VV. Thyroid function in men taking carbamazepine, oxcarbazepine, or valproate for epilepsy. Epilepsia. 2001;42(7):930-934. doi:10.1046/j.1528-1157.2001.042007930.x
- Sodium salicylate and synthroid interactions. Drugs.com. https://www.drugs.com/drug-interactions/sodium-salicylate-with-synthroid-2094-0-1463-869.html. Accessed October 14, 2021.
- Gamstedt A, Järnerot G, Kågedal B, Söderholm B. Corticosteroids and thyroid function. Different effects on plasma volume, thyroid hormones and thyroid hormone-binding proteins after oral and intravenous administration. Acta Med Scand. 1979;205(5):379-383.
Note: Originally published in August 2015, this article has been revised and updated for accuracy and thoroughness.